Sacroiliac Joint Dysfunction Review
Sacroiliac Joint Dysfunction and Anatomy
What is the Sacroiliac Joint Made Of?
The sacroiliac joint (SIJ) is composed of both fibrocartilage and hyaline cartilage. The fibrocartilage is found lining the iliac side, and the hyaline cartilage lines the sacral side, both of which are encapsulated by a fibrous capsule. The SIJ is a diarthroidal synovial joint with an anterior segment (true synovial joint), and a posterior segment. The posterior segment is a syndesmosis that is composed of the gluteus minimus and medius, piriformis, and sacroiliac ligaments. Since all these muscles are shared with the hip joint, the SIJ cannot function independently. The SIJ serves to provide stability, is a C-shaped joint, and has two interlocking lever arms at the S2 level. The stability of the SIJ is boosted by the large number of surrounding ligaments. The ligaments are the deep anterior, posterior, and interosseous ligaments which all resist the load of the sacrum relative to the ilium. The superficial ligaments are the sacrotuberous, long and short sacroiliac ligaments, all of which react to dynamic motion. The long dorsal ligament can be stretched in periods of reduced lumbar lordosis.
Can This Joint Be a Low Back Pain Generator?
Dysfunction in the sacroiliac joint is associated with hyper- or hypo- mobility with low back pain or pelvic girdle pain. Sacroiliac dysfunction is mostly a diagnosis of exclusion, and thus other conditions must be ruled out first through a thorough physical assessment. SIJ dysfunction is a common cause of low back pain, occurring in 16-30% of low back pain patients. There are many causes that lead to sacroiliac joint dysfunction. They include a direct fall or trauma that causes pelvic rotation, asymmetrical motion of the pelvis (leg-length discrepancy, scoliosis, unilateral weakness, unilateral weight bearing pain), asymmetrical laxity of SIJ during pregnancy, abnormal gait, hip or knee osteoarthritis (which can lead to leg-length discrepancies), repetitive trunk and hip rotation, and inflammatory arthritides. The pain generators are believed to be the SI joint ligaments and the SIJ surface. Due to the high innervation of the SIJ, many referral patterns are possible and it may be the source of groin and thigh pain. Aggravating factors include stair climbing, car transferring, and transitioning from sit-to-stand.
What Are The Risk Factors?
Risk factors for this condition include age over 50 years, female gender (due to broader pelvis, greater femoral anteversion, and shorter limb lengths), sports (involving throwing, kicking, and unilateral loading), pregnancy, scoliosis, trauma, lumbar fusion surgery with fixation of the sacrum, history of recurrent back pain, and heavy workload occupation.
What Are My Treatment Options?
Treatment for SIJ dysfunction is vast and include repetitive exercise, joint mobilizations, manipulation, bracing, massage, patient education, aerobic conditioning, general therapeutic exercise, electrotherapeutic modalities, heat, ultrasound, and TENS. A systematic review revealed that exercise, manipulation, and kinesiotaping were the most effective at reducing pain, disability, and restoring normal pelvic symmetry in patients, and among these manipulation was favored. Chiropractors are known to be adept practitioners of manipulation but some physiotherapists are also trained to perform this maneuver. Consult either type of therapist for a physical assessment to see which treatments are best for you. Registered Massage Therapists can also help with massaging out tight muscles and to reduce muscle tension. At the Rehab Hero clinic, all types of practitioners are trained to give you an exercise program for long lasting results.
Which Tests are Used to Diagnose Sacroiliac Joint Dysfunction?
After ruling out other conditions, your chiropractor or physiotherapist may perform other orthopaedic tests to diagnose this condition. Some tests include:
Thigh Thrust
Sacroiliac Joint Shear
Sacroiliac Joint Lateral Compression
Sacroiliac Joint Open Book or Distraction Test
Posterior to Anterior Sacral Compression
In most instances diagnostic x-ray, ultrasound, MRI, or CT scan is not required to make a clinical diagnosis.
What Are The Differential Diagnosis?
Differential diagnosis are diagnosis that present similarly to the actual diagnosis. Due to the ever changing nature of signs and symptoms, these differentials are often revisited during follow up appointments to confirm that you are on the correct treatment plan. If follow ups reveal that new signs or symptoms are gearing towards a differential, this gives your clinician or therapist an opportunity to adapt your treatment plan accordingly. Some differential diagnosis include:
Piriformis Syndrome
Lumbar Facet Syndrome
Thoracolumbar Syndrome
Proximal Gluteus Maximus Tendinopathy
Proximal Hamstrings Tendinopathy
Be sure to consult your health care practitioner in person or online about any inquiries about your current diagnosis. Virtual Telehealth Appointments can be completed to assess and diagnose these conditions. Do not self diagnose as a treatment plan for one differential diagnosis may aggravate your pain for another diagnosis.
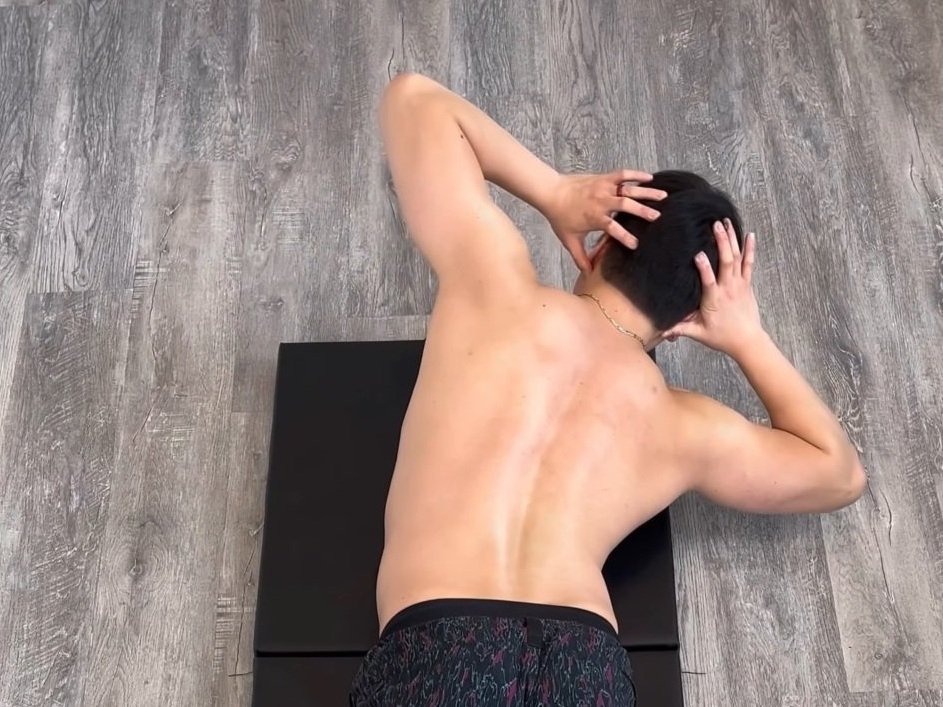
What Are Some Exercises for the Sacroiliac Joint?
Exercises may vary depending on your physical assessment and movement competency. Exercises can be done to directly work on the stabilization of the sacroiliac joint, however be sure to be properly diagnosed to discover the root cause for the dysfunction. Your chiropractor or physiotherapist will be able to evaluate you through movement screens to understand how your hip, knee, ankle, back, or core function relates to your sacroiliac joint pain. Here are a few basic stability and strengthening exercise options for building stability through the sacroiliac joint:
DISCLAIMER: The information in this blog post is not intended nor implied to be a substitute for professional medical advice, diagnosis or treatment. All content, including text, graphics, images, and information, contained in this video is for general information purposes only and does not replace a consultation with your own doctor/health professional.
Here is a 10 minute video on steps that you can take when it comes to recovering from sacroiliac joint syndrome:
References
1. Matlick D, Dressendorfer R. Sacroiliac Joint Dysfunction. CINAHL Rehabilitation Guide [serial on the Internet]. (2017, Sep 22), [cited November 13, 2017]; Available from: Rehabilitation Reference Center.
2. Al-Subahi M, Alayat M, Alshehri M, Helal O, Alhasan H, Alfaqeh A, et al. The effectiveness of physiotherapy interventions for sacroiliac joint dysfunction: a systematic review. Journal Of Physical Therapy Science [serial on the Internet]. (2017, Sep), [cited November 13, 2017]; 29(9): 1689-1694. Available from: MEDLINE with Full Text.