Lumbar Segmental Instability
Why does my low back hurt?
Learn about one of the reasons why you may be experiencing low back pain.
What is lumbar instability?
Lumbar instability refers to the loss of normal biomechanical function between two levels of adjacent vertebrae. This leads to increase abnormal motion, static malposition, or decreased joint proprioception. This can be caused by true instability due to laxity in connective tissues, or functional due to joint proprioception loss.
Ligament and muscle laxity can result increased motion which is also known as hypermobility. This can occur as a result of compensational movement for hypomobile joints (joints with decreased motion). In this case, joint hypermobility can result secondary to soft tissue contractures, scar tissue adhesions, or reactive muscle guarding.
It is currently believed that there are four types of instability.
Segmental Instability
This refers to a single segment of hypermobility that is compensating for an adjacent hypomobile segment. This type of instability is reversible when hypomobile segments are addressed (decreasing the need for compensation at the hypermobile segment).
Functional Instability
This type of instability refers to dysfunctional coordination between antagonist and agonist muscles. Joints require opposing muscles to co-contract in order to maintain maximally joint centration. When dysfunctional, momentary sharp pain may be experienced mid-movement, and will often disappear when continuing to push through the movement to completion. This type of instability may be recurrent and is the result of muscle imbalance. This type is reversible with exercise conditioning and proprioceptive retraining.
Structural Instability
This type of instability is due to the result of ligamentous damage, often as a result of acute trauma. With this type of instability pain is often experienced at the end-ranges of movement. Stress x-rays may show increased range of motion in flexion and extension views. This type of instability is difficult to reverse and often requires long term functional conditioning of the spinal stability muscles.
Surgical Instability
Similar to structural instability, this type of instability is due to the result of ligamentous damage, often resulting from an acute injury. This type of instability is very instable and will require surgery. Examples of this type instability include a grade III ligament sprain or progressive spondylolisthesis.
What does lumbar instability feel like?
Lumbar instability can produce recurrent dull, achy low back pain. A catching pain may be experiencing during lumbar flexion movements, at mid range or end range, or returning from flexion to neutral. The pain is often better with rest or while using support. Pain is relieved with joint mobilization or manipulation but relief tends to be temporary, with pain recurring a few days later without requiring an aggravating trigger. Patients may sometimes report that their back ‘feels out’ or ‘not quite right’ particularly during lumbar flexion activities (such as trying to put on a pair of socks, shoes, or when bending over to pick something off of the floor).
Who does lumbar instability affect?
Lumbar instability can occur at any age, often ranging from 15-50 years old. This condition does affect females more than male and there may be a genetic component to it. Repetitive work or sport action may predispose someone to lumbar instability injuries. Other risk factors include:
Previous dislocation, subluxation and or injury
Participation in flexibility based sports such as gymnastics or ballet
Wearing high-heels (leading to hyperlordosis)
Muscle deconditioning
Congenital ligament laxity (Elhers-Danlos Syndrome, Marfan’s Syndrome)
Do I need an x-ray to get a diagnosis?
For non-acute injury based lumbar instability an x-ray or other diagnostic imaging will not be required. As previously mentioned, a stress x-ray in lumbar flexion or extension may be taken if ligamentous laxity is suspected as the result of trauma. X-rays may also be recommended for the assessment of spondylolisthesis, but can be recommended following a physical examination with your a chiropractor or physiotherapist near you.
Clinically, orthopedic tests can be used for the assessment of lumbar instability. Tests such as the bilateral leg raise, Goldthwait’s test, nerve tension tests, sit-up arc test (Farfan compression test), among others may be used to diagnose your condition.
What types of treatment help?
Massage therapy, joint mobilization, or joint manipulation may be used for symptom management in the short term. Massage therapy and joint mobilizations can be provided by your registered massage therapist, physiotherapist or chiropractor. Joint manipulation may be provided by your chiropractor or certified physiotherapists.
It is important to recognize that the aforementioned manual therapy will only provide short term relief for non-surgical lumbar instability. Additionally, it is important to keep in mind that functional conditioning of the lumbar muscles will be required for long term results. Exercise rehabilitation should be programmed to mobilize hypomobile lumbar segments, and to stabilize hypermobile segments. Proprioceptive retraining of the trunk and lower limbs will also be required to minimize recurrent pain. Exercise programs can be provided by experienced RMTs, physiotherapists and chiropractors
To book in with a Rehab Hero clinician in Markham or Toronto, click the button below:
What are some examples of exercises for lumbar instability?
Exercises focusing on core endurance and proprioceptive feedback will be important to improve functional lumbar stability.
An exercise example for core endurance is the Bear Crawl Hold:
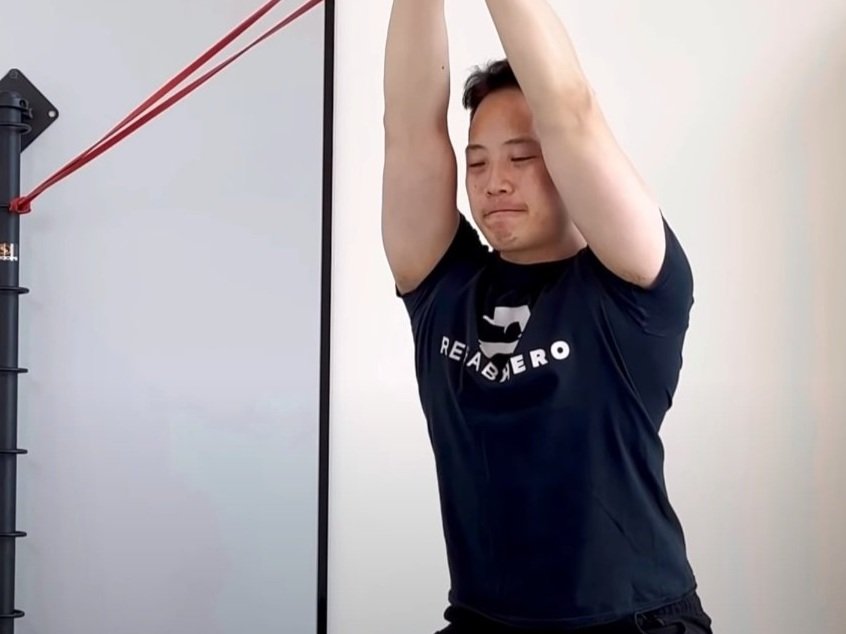
An exercise example for lumbar proprioception is the Hip Hinge Pallof Press:
For additional exercise programming it is recommended to ask your health care team for exercises that are individualized to your current level of fitness.
Written by:
Dr. David Song, Chiropractor, Acupuncture provider, Rehab coach